Pain is not a single experience so much as a collection of signals, ideas, and behaviors that merge at the worst feasible time. In prehospital and emergency settings, that intricacy gets here with flashing lights and high risks. PUAEME008 Provide Discomfort Administration exists for that truth. It equips responders, nurses, and allied wellness professionals with sensible, evidence-based tools to evaluate discomfort precisely, treat it securely, and supporter for patient comfort without endangering clinical priorities.
I have spent lengthy changes pacing the narrow aisle of ambulances, negotiating morphine doses while the road thrown under our wheels, and fielding concerns from distressed family members that wanted reassurance greater than pharmacology. I have actually additionally viewed pain spiral past physiology and bleed right into panic, dispute, and loss of depend on. The abilities in the give pain management training course do greater than lower a number on a range. They shape outcomes, reduce problems, and make treatment feel humane.

What this system covers and who benefits
PUAEME008 Offer Discomfort Management is identified across emergency services and commonly ingrained suffering management training for nurses, paramedics, and -responders. It concentrates on fast assessment and purposeful treatment, with an equilibrium of medication and non-drug strategies. Graduates should have the ability to determine the system of pain, choose a secure alternative from the local formulary or concurred protocols, supply it with suitable surveillance, and assess feedback in real time. The purpose is decisiveness without carelessness, convenience without oversedation.
Many learners approach this as part of wider discomfort management training programs or as one of numerous brief courses in pain monitoring to update abilities. It rests well alongside a certificate program in pain administration or a pain administration qualification course that goes deeper into persistent discomfort, neuropathic mechanisms, or interdisciplinary planning. For medical professionals in intense treatment, specifically those looking for a discomfort administration certification concentrated on emergency discomfort management, PUAEME008 is practical and instantly applicable.
If you work in health center triage, country retrieval, occasion medication, or area urgent care, the frameworks translate directly. Discomfort monitoring training courses for registered nurses and discomfort management training courses for physiotherapists typically attract from the very same evidence base however vary in range and authority to administer medicines. Understanding where PUAEME008 starts and where various other competencies take control of aids produce a systematic plan of treatment rather than a jumble of good intentions.
The attitude behind reliable discomfort management
Good pain care is much less about remembering dosage tables and more regarding routines of thought. The best clinicians share a couple of traits. They are curious concerning the mechanism of pain, humble about uncertainty, and disciplined with review. They match treatment to cause, instead of going after a number. They comprehend that patient count on is an effective analgesic in its very own right.
In practice, that suggests you do not treat a broken thigh with the same toolset as a migraine mood or biliary colic. It additionally indicates you withstand restorative inertia. If a treatment stops working to move the needle by a minimum of two points on a practical range, you pivot or escalate under method. And you document the story of the pain as thoroughly as the interventions, since context overviews your adhere to through.
An anecdote enters your mind. A teenager with a suspected ankle crack was available in after a netball video game. Her discomfort score was 8, but her breathing was stable and she was chatting with close friends. We picked ice, altitude, immobilization, and a timed dosage of dental analgesia en course to imaging. She went down to a four prior to X-ray and never required opioids. The trick was not blowing. It was confidence in pathophysiology and ideal non-opioid actions. PUAEME008 instructs that sort of stable judgment.
Assessment: the backbone of the unit
If you only take one thing from the provide discomfort management course, take the discipline of organized assessment. Discomfort is subjective, yet its context is not. System of injury, time since start, place, radiation, linked signs and symptoms, exacerbating and easing factors, and functional effect, these pieces develop a picture you can treat.
Adult clients can generally engage with a numerical ranking range from 0 to 10, yet you must customize the technique. Some react better to a verbal descriptor scale with options like mild, moderate, severe. For kids or those with cognitive disability, a faces range or behavioral hints might be a lot more significant. I have discovered to deal with outliers with caution. A calm farmer gritting his teeth at a 3 can be in more problem than a talkative urbanite at an eight with regular vitals. Respect the number, yet do not follow it blindly.
Vital signs issue. Tachycardia and high blood pressure can be discomfort, worry, hypovolemia, or blood poisoning. Respiratory price is essential when you take into consideration opioid titration. Oxygen saturation, capnography if readily available, and pupillary size help spot sedation and impending hypoventilation early. For localized injuries, a focused examination with palpation, neurovascular checks, and range of activity offers targets for regional blocks or splints. For natural pain, believe pattern acknowledgment. Right upper quadrant pain after a fatty meal factors you towards biliary colic. Colicky flank discomfort with hematuria recommends kidney stone. These distinctions guide whether you lean on NSAIDs, antispasmodics, or titrated opioids.
Analgesic pharmacology in the field
Local methods vary, so I will speak in concepts as opposed to a fixed drug checklist. PUAEME008 Give Discomfort Management stresses understanding start times, peak results, duration, and negative effects profiles, and matching those to the environment.
Oral paracetamol is essential. It is secure at healing doses, synergistic with NSAIDs, and helpful as a background agent also when you prepare to escalate. In injury with threat of blood loss, NSAIDs require caution. If you have no contraindications, they supply solid relief for musculoskeletal discomfort and renal colic. For opioids, tiny titrated doses defeat bolus application in dynamic settings. Aim for incremental doses with clear targets and necessary reassessment. You do not chase after absolutely no pain when the device is major and the transport is brief. You go for bearable, workable feature and very little unfavorable effects.
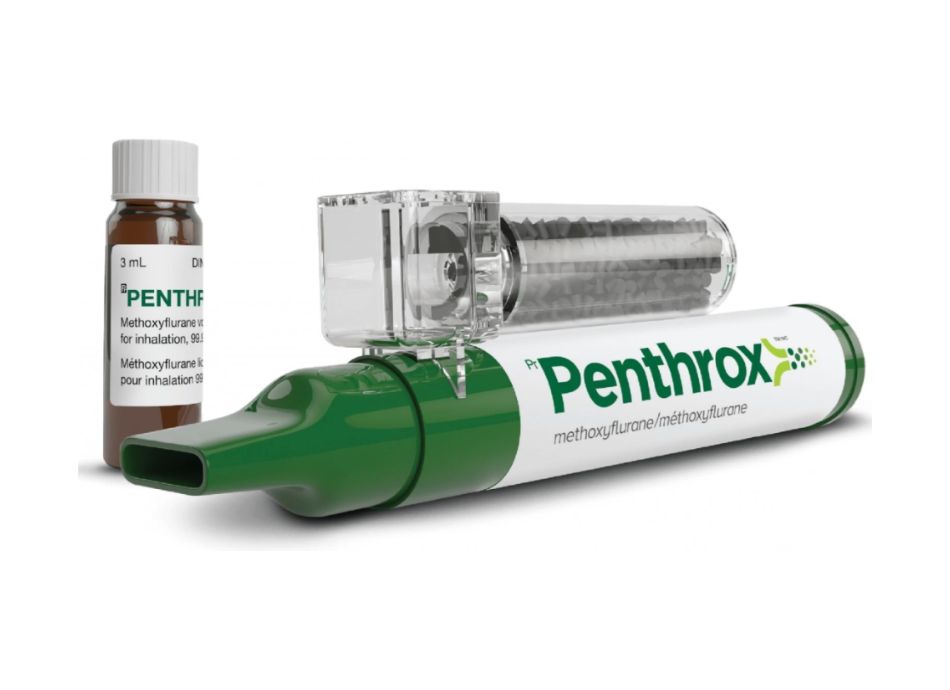
Ketamine is entitled to an area in emergency pain management when protocols sustain it. At sub-dissociative dosages, it supplies analgesia with much less respiratory clinical depression than opioids. It can cause dysphoria or nystagmus, so prepare the client with a simple description and a tranquil setting. Laughing gas serves for short treatments if you have scavenging and qualified personnel. It is not optimal for patients with pneumothorax, bowel blockage, or recent diving. Anesthetics for local strategies, such as an ankle block or a fascia iliaca block, can transform a transport. They require training, clean and sterile strategy, and physiological self-confidence. When succeeded, they decrease opioid usage, support vitals, and enhance safety.
The supply discomfort monitoring course does not transform learners right into anesthetists. It instructs you to choose the least dangerous efficient alternative within your authority. If your range permits only dental or intranasal representatives, learn them deeply. Intranasal fentanyl has useful benefits in people with bad IV accessibility, specifically kids. Onset fasts, application is foreseeable, and surveillance is necessary. With any type of opioid, prepare for queasiness and consider treatment when suitable. Maintain regard for variability, specifically in older grownups, those with kidney or hepatic disability, and clients on sedative medications.
Non-pharmacological approaches that actually work
It is simple to disregard non-drug methods as window dressing. That is a blunder. In the confined rear of an ambulance or a resus bay with alarms tweeting, simple procedures can shave two points off a discomfort score prior to you split open a vial.
Immobilization and splinting are one of the most effective. A well-fitted vacuum cleaner splint on a suspected tib-fib crack lowers activity and isolates discomfort. In shoulder dislocations, a sling complied with by mild, protocolized reduction under analgesia brings back convenience and feature. Cold packs for intense soft cells injuries and burns, warm packs for muscle mass convulsion, both have their location. Elevation decreases swelling. For kidney colic, antispasmodics and warm sometimes make the distinction between writhing and quiet.
Breathing techniques and distraction sound soft up until you see them work in youngsters. A bubble wand, a concentrate on counting breaths, or a brief narration script can deflect interest enough time for intranasal analgesia to begin. For adults, calm explanations lower anxiety. I commonly narrate what I am doing, in plain language, and request feedback. The patient ends up being a companion, not a passive recipient. Their feeling of control lifts, and discomfort slows its hold.
Monitoring and safety: what divides proficiency from luck
Any pain administration certification worth its charge strengthens surveillance as a non-negotiable. The drug is the very easy component. The repercussions reside in the mins that comply with. Pulse oximetry, breathing rate trending, psychological condition checks, and, where readily available, capnography, form your safety net. After an opioid dosage, I assign somebody to watch the chest and the face while I chart or prepare the next step. Search for slowing, shallow breathing, new snoring, or a glazed look. If capnography rises over expected baselines, act early.
Reassessment ought to be structured. Document the pain rating, functional condition, and vital indications at agreed intervals, generally every 5 to 10 mins after titration or step-by-step actions. If the setting is disorderly, utilize a psychological list: pain, pressure, pulse, students, pattern of breathing. Change the plan when the trajectory is incorrect. Add antiemetics for queasiness. Slow down or quit if sedation creeps up. Never ever press an opioid to zero pain prior to a step-by-step sedation unless your team and tools are ready for airway management.
Adverse results belong to the landscape. Opioid-induced nausea and pruritus prevail, as is hypotension in volume-depleted clients. Ketamine can elicit affective changes, workable with confidence and lowering ecological stimulations. NSAIDs intensify gastritis and threaten kidney function in vulnerable people. Paracetamol overdosing is uncommon in trained hands but unrelenting, so calculate overall everyday dosage throughout all resources. The pain administration training for registered nurses specifically drills these details, because they often come to be the cautious eyes at the bedside when prescribers move on.

The subtlety of special populations
Older grownups metabolize drugs in a different way, and their reserve is thinner. I begin low and go slower, then stop briefly to view. Frailty frequently masks pain expression. A quiet elder with a hip crack may remain in misery however as well tired to report it. Dosages that barely touch a healthy thirty-year-old can snow a ninety-year-old on a beta blocker. Useful goals need to steer the plan. Can they endure gentle repositioning, imaging, or transfer without distress?
Pediatrics flips the script. Weight-based application, intranasal courses, and fast-onset options power. Fear is half the battle. A positive, warm strategy, combined with topical anesthetics for IV placement and intranasal fentanyl or ketamine where licensed, transforms a spiraling scene into a controlled one. The discomfort administration programs for registered nurses who staff pediatric devices emphasize uniformity and parent mentoring. Welcome the moms and dad to help with positioning or distraction. Stay clear of restraining kids unless security demands it.
Pregnancy complicates points. NSAIDs are typically avoided in later trimesters. Opioids can be utilized with care for intense indications but call for counseling and judicious application. Regional techniques that bypass systemic direct exposure might be suitable. For clients with chronic opioid usage or dependence, established expectations early. Do not keep analgesia as a result of stigma. Use multimodal non-opioid representatives, consider ketamine where appropriate, and titrate opioids to result with clear monitoring.
Procedural pain and the value of preparation
Procedural pain is foreseeable. Cannulation, breast drains, reductions, and injury treatment all harmed in details ways. Planning defeats improvisation. If a reduction is required, pre-brief the team. Appoint roles. Pick analgesia and anxiolysis that match the period and strength. For brief, sharp treatments, laughing gas or intranasal representatives can be sufficient. For longer jobs, think about regional blocks or a thoroughly kept an eye on sedation supplied by skilled personnel. The distinction between a smooth moving and a traumatic one usually lies in the added 2 mins spent discussing the actions to the individual and applying a targeted block.
I once utilized a fascia iliaca block for a highway fall patient with a believed femoral crack. We had a lengthy extrication and longer transport. With ultrasound and sterilized technique, the block established within 15 mins. His heart price settled, and the ride changed. Nothing brave, simply disciplined application of learned skills.
Documentation that tells the real story
A pain administration certificate course rightly hammers the pain management courses significance of documents. Not because paperwork matters greater than patients, however due to the fact that a clear document protects them and you. Record the first discomfort assessment, treatments with precise timing and doses, reassessment results, adverse effects, and individual preferences. When the tale is unusual, create the reasons. If you withheld NSAIDs because of renal disease, say so. If you picked intranasal over IV because of inadequate gain access to and patient distress, note it. This narrative ends up being the handover's foundation, permitting continuity in the emergency division and beyond.
Building proficiency with calculated practice
The PUAEME008 Supply Discomfort Monitoring device is a starting factor, not a finish line. Abilities degeneration without usage. After program conclusion, seek circumstances that extend you under guidance. Practice landmarking for regional methods on associates in simulation. Time your beginning and peak results in training drills. Debrief after genuine cases that worked out and those that did not. What did you miss? Where did you wait? Did you reassess as commonly as you planned?
Pain monitoring training programs that include simulation with actual screens, capnography, and patient stars change concept into muscular tissue memory. Pain monitoring certification programs for registered nurses and allied health staff that incorporate expertise sign-offs and supervised scientific changes deserve the investment. Short courses suffering monitoring that concentrate on a single domain, such as ketamine analgesia or nerve blocks, can sharpen a targeted skill without overwhelming schedules.
Navigating methods and autonomy
Protocols secure individuals and clinicians. They systematize secure practice and lower uncertainty under pressure. Yet, rigid adherence without clinical thinking can backfire. A method may allow 5 to 10 mcg intranasal fentanyl in a youngster, repeated at taken care of periods. If the child comes to be sluggish after the very first dosage, repeating it just because the clock allows it is bad care. Alternatively, withholding a dosage in a yelling youngster with intact respiratory tract reflexes and a displaced crack because the pain rating has not been come back yet is additionally bad care.
This is where PUAEME008's focus on assessment and reassessment issues. You document the discrepancy with clear thinking. You confer with medical control when called for. You keep the person, not the type, at the center of choice making. Gradually, you will discover where your service's discomfort management training motivates adaptability and where it demands strict sequence.
Measuring what matters
Pain ratings are one statistics. Functional goals are much better. Can the client take a deep breath after you handle rib cracks? Can they exist still for imaging? Can they participate in a neuro test without wincing at every touch? These are scientifically significant gains. When you communicate these in handover, you direct the following team's choices. You additionally track the trajectory. A client whose pain keeps rising despite escalating analgesia needs a new medical diagnosis or a new strategy, not simply an additional ampoule.
From a system point of view, services that buy a supply pain management course and refresher courses see downstream advantages: fewer ED accelerations for anxiety, smoother imaging flows, reduced sedation prices for minor procedures, and higher client fulfillment. These are concrete results. They likewise minimize staff fatigue. It is wearying to watch someone experience when you understand you can help.
When discomfort is a carrier, not a target
Not all discomfort ought to be completely reduced. Abdominal discomfort with peritonism in an unpredictable person requires examination together with analgesia. We are past the period where opioids rare medical indications past utility, however we still value the body's cautions. In compartment disorder or progressing spine compression, discomfort guides us towards early intervention. The lesson is subtlety, not nihilism. Treat discomfort, monitor closely, and stay alert for discordant findings that suggest a more hazardous process.
Similarly, in head injury, focus on modifications after analgesia. Enhanced convenience is great. New complication is not. Sedation and hypoventilation can masquerade as renovation to the unwary. Support on your own with objective information and maintain pain management course an examining mind.
Professional growth pathways
Clinicians commonly ask whether they should go after a discomfort administration certification beyond the system. The answer relies on duty and passion. For numerous in EMS or acute treatment nursing, PUAEME008, coupled with normal inner drills and procedure updates, supplies the appropriate degree of competence. For those intending to lead policy or teach, a wider pain administration certification program or a certification course suffering management that covers persistent discomfort, biopsychosocial models, and interdisciplinary treatment might be beneficial. Physiotherapists who intend to develop acute techniques can pick discomfort monitoring programs for physio therapists that highlight regional technicians and non-pharmacological approaches in the first 72 hours after injury. Registered nurses in EDs benefit from discomfort monitoring training for registered nurses that codifies triage analgesia, nurse-initiated methods, and interaction skills for distressed families.
When contrasting discomfort administration training programs, search for real-time situation method, professors with frontline experience, clear range positioning with your authority, and a prepare for preserving competence in time. Stay clear of programs that promise miracles or rely upon filler material. You will certainly find out more from three hours of severe simulation than from a loads slides read aloud.
A succinct field list for PUAEME008 skills
- Assess system, place, intensity, and useful effect. Capture vitals, warnings, and patient expectations. Choose an evidence-based intervention within scope. Pair non-drug procedures with a first agent fit to system and risk. Administer thoughtfully. Titrate in little increments, describe the strategy, and prepare for damaging effects. Monitor and reassess. Track pain, function, and physiology. Adjust or rise based upon reaction, not inertia. Document decisions and outcomes. Connect the story of the discomfort and the results of your interventions at handover.
The human element
The first minutes with a person usually figure out the remainder of the encounter. Present yourself. Ask what injures most, not simply where. Repeat back what you hear. Offer choices where feasible. Would you like to attempt a nasal spray for fast relief while we obtain you more comfy for the trip? Lots of people state yes when they really feel respected.
I assume usually of a night on a country road where a woman with a clavicle crack sat stiff with fear. Our supply was limited. We provided intranasal fentanyl, applied a sling, and utilized a gentle block at the crack's community after reviewing threats. We dimmed the lights in the back and kept discussion soft. Her pain went down from nine to 4. She oversleeped snatches on a lengthy drive and thanked us except the medicines, but for the tranquility. That is the core of PUAEME008 offer pain monitoring. It is a framework to develop tranquil where disorder intends to win.
Pain monitoring is not about heroics. It has to do with taking care of detail, valuing physiology, and staying existing. With the ideal training, including a concentrated provide pain administration training course and, where pertinent, a wider pain administration qualification, you can supply treatment that is risk-free, swift, and deeply humane. The evidence sustains these methods. A lot more significantly, patients remember them.